DKA: Let's Get Cellular
- joshishmael85
- Jul 1, 2024
- 3 min read
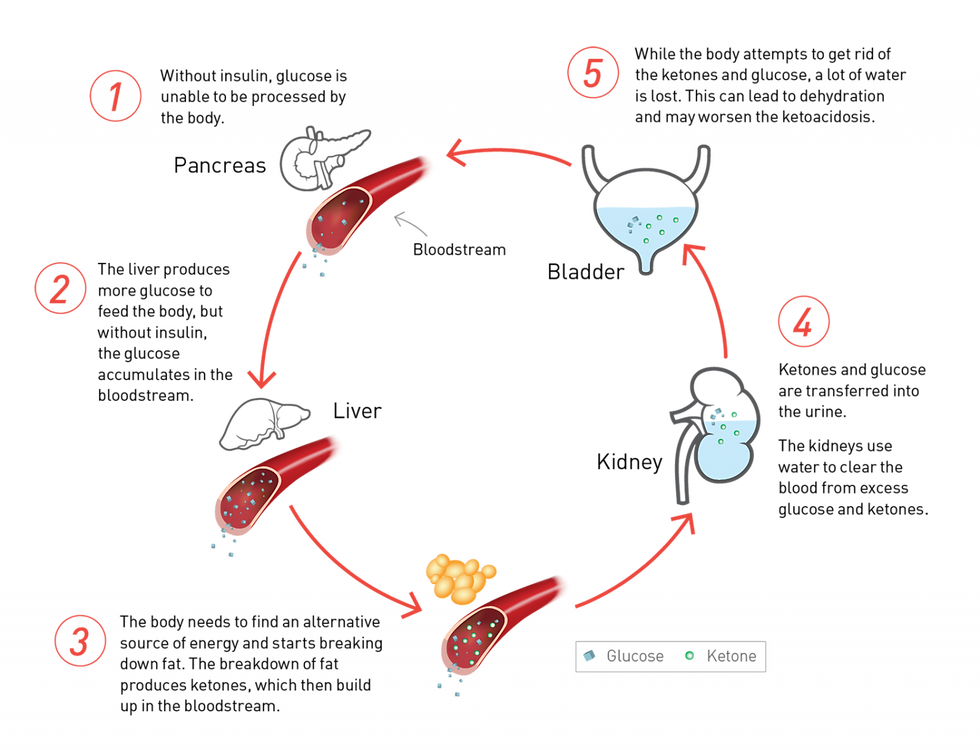
Diabetes and its associated complications continue to run rampant across this country. The reasons why are multifactorial, and we won't get into those discussions here. During this week's blog we will chat about the significant illness that insulin dependent (Type I) diabetics may be up against: Diabetic ketoacidosis (DKA). Many times, these events will require EMS intervention and lengthy hospitalizations. On a broad scale these patients make little to no insulin. Think of insulin as the vehicle that allows glucose to travel from the bloodstream into the cells. As you can imagine without this hormone glucose metabolism is altered or even absent. Therefore, it tends to stack up in the bloodstream. We now encounter two issues: the patient is profoundly hyperglycemic, and the cells are starving because their main source of fuel is missing.
This triggers another mechanism in which the cells look for and break down an alternative fuel source: fat. The subsequent metabolism of these fats causes ketone production. By their very nature these breakdown products (BHB, acetone, acetoacetate) are acidotic. This point allows me to pause and reinforce the fact that the high glucose isn't the killer -- the drastic pH derangement is what contributes more to their demise. The ketones outnumber our body's ability to act as a buffer and maintain homeostasis. The acute treatments are focused on reversing the acidosis and replacing their intravascular volume. The mechanisms are simplified in the illustration below:
The patients themselves will often try to correct/compensate for the metabolic acidosis by creating a transient respiratory alkalosis. You may recall this as Kussmaul respirations. They are unusually deep, regular and rapid in nature and help blow off excess CO2 from the body. Additionally, DKA is not treated by insulin alone - fluid resuscitation and rehydration must also occur in a complimentary fashion. Some of these patients have a tendency on ED arrival to be hyperkalemic as well. After we fill up the tank, and the physician starts the insulin the potassium levels will also begin to come down and normalize. In the rarer event they may arrive in a hypokalemic state, in this case it is paramount that the electrolyte be replaced before the insulin drip starts. Insulin causes glucose to shift (that's what we want) but it also causes potassium to shift as well.
I want to draw a contrast to another diabetic complication seen in Type II patients. These folks are not insulin dependent, but their bodies become insulin resistant. Because insulin is still present, they will not produce ketones, and therefore will not become acidotic. They are suffering from HHS or HHNK. This may take weeks to fully manifest and BGL levels can approach 2,000 mg/dl. It is important to note that their mortality rates are much higher here as compared to DKA. This is likely because HHS tends to target older patients who have other co-morbidities. You will also find that the volume depletion from osmotic diuresis is also much worse in these cases. Another key difference in the laboratory is the anion gap [Na+K - Cl+HCO3]. In DKA the gap will be high, whereas in HHS the gap could be variable or even non-existent. A brief differentiation summary is outlined here:
To close out, it is important to note that about 20% of patients with Type I diabetes admitted for DKA will be readmitted for DKA within 30 days. Several studies suggested that the omission of insulin is one of the most common precipitating factors of DKA, sometimes because patients are socio-economically underprivileged, and may not have access to or afford medical care. The costs of insulin has been the subject of much debate in many political arenas as of late. Reducing the costs of these drugs will go a long way in removing barriers to treatment and allowing for better prevention measures.
Close follow up is very important, as it has been shown that monthly check-ins can reduce the number of ER admission for DKA. This patient demographic could be one such example (in addition to others) where the utility and deployment of a community paramedic program may provide some great value and reduce the burden on the already taxed healthcare systems.
July 1, 2024
Author: Joshua Ishmael, MBA, MLS(ASCP)CM, NRP
Pass with PASS, LLC



Comments